It has been more than a year since the global roll-out of COVID-19 vaccines, yet the gap in vaccination rates between high- and low-income countries continues to grow. Supply shortages are no longer the primary issue, with logistics challenges and vaccine hesitancy emerging as the main barriers to uptake in many low-income countries.
Among an “infodemic” of abundant and potentially harmful misinformation about COVID-19, people already suspicious of the vaccine’s origins are drawn to information that seemingly confirms their beliefs and can be resistant to new and contradicting information. Even if few people believe conspiracy theories, they contribute to a cloud of uncertainty about the vaccine and possible adverse side effects. This undermines the public health response, fomenting mistrust of governments’ priorities and motivation, as well as suspicion about foreign actors’ involvement in pushing vaccines.
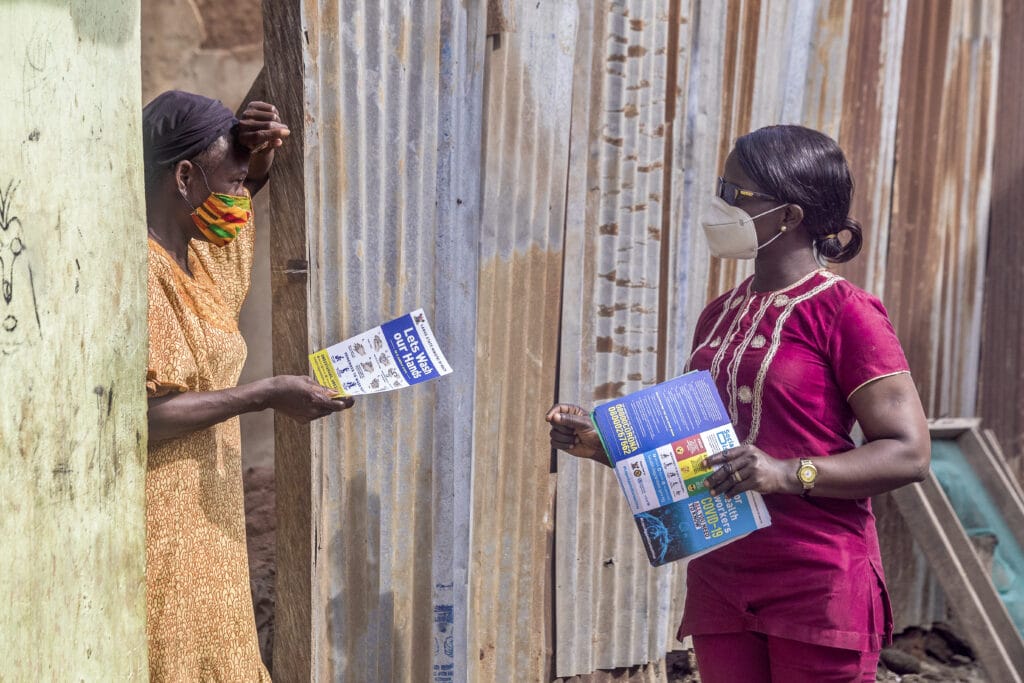
As part of the USAID-funded Breakthrough ACTION project, we are working with teams and governments in eight countries—Liberia, Côte d’Ivoire, Cameroon, Senegal, Mali, Burkina Faso, Philippines, and Nigeria—to understand and target demand-side barriers to improve acceptance and uptake of the COVID-19 vaccine. Our formative work has explored the context surrounding vaccine-related decision-making and behavior in each country through interviews with healthcare workers and community leaders, as well as the general public.
Below are three cross-cutting behavioral insights from our initial work across Liberia, Côte d’Ivoire, and Cameroon that suggest opportunities to encourage uptake in low-resource settings despite persistent challenges to vaccine acceptance.
Opportunity #1: Make peer vaccination more visible
Despite widespread exposure to misinformation, we found that seeing a peer or someone you identify with safely vaccinate can be a powerful driver towards personal acceptance. In some cases, this can serve to directly counter beliefs—for example, seeing that a friend who got vaccinated is now pregnant can help to overcome misinformation-related concerns about infertility. In other cases, someone may feel compelled to accept the vaccine after seeing others do so, even if they still harbor personal concerns or uncertainties. Whether peer vaccination effectively counters or simply trumps negative beliefs, this observation suggests that normative interventions to increase the visibility of vaccine uptake among peers can help drive demand, even without more intensive belief-shifting efforts. It also underscores the importance of making vaccines easily accessible to those already motivated to receive them, as their actions may have a downstream impact on their peer network.
“When the boss gets vaccinated, I stay without getting vaccinated—why? I said, ‘vaccinate me.’ If it did something to you it will do something to me.” – Community member, Cameroon
“I took the vaccine because I saw some of my friends who took the vaccine moving around smoothly.”– Provider, Liberia
Opportunity #2: Prime identities
We observed that one’s perceived status as a role model or desire to set a good example can help to override personal doubts about the vaccine among community leaders and health workers. We found examples of this responsibility either driving personal vaccine uptake or at least leading to a willingness to promote vaccination to others through their capacity as a community leader, even if they remained hesitant themselves. This suggests that prompting people to consider aspects of their identity that would also align with setting a good example with regards to vaccines, such as informal roles within family and friend networks, might help build more inroads into hesitant communities, in addition to leveraging local influencers.
“They themselves are taking the vaccine because we the health workers are the example, and the people look up to us. So, we are serious about the vaccine…” – Provider, Liberia
“…For someone to come and be vaccinated, I had to be vaccinated to motivate the population. When we went to the community, you had to be the model, the example.” – Provider, Cameroon
Opportunity #3: Communicate other downsides to staying unvaccinated
Finally, more recent emerging evidence suggests that anticipation of future hassles related to one’s unvaccinated status can increase the perceived urgency of getting vaccinated and willingness to do so among those otherwise on the fence or ambivalent. Several people we spoke to cited restrictions against traveling across borders, entry into government buildings, or future work requirements as reasons they expected to take the vaccine. This suggests that vaccine mandates for specific activities that people want to engage in could be a potentially effective tool in these settings, as they have been found elsewhere.
“Crossing borders, they say, ‘Ah, you didn’t get the vaccine, you can’t go into such and such a country…’ So, it’s better to get vaccinated.” – Provider, Côte d’Ivoire
“You have to get vaccinated if you want to go to France…But if I don’t see this obligation, I’m in no hurry.” – Community member, Cameroon
Vaccine uptake is as much a behavioral problem as it is logistical, and our early insights in Liberia, Côte d’Ivoire, and Cameroon suggest opportunities to encourage vaccination that may resonate across other settings facing similar behavioral challenges. We believe such insights can be leveraged through behavioral design and will play an important role in boosting vaccine uptake efforts and reducing the vaccination disparity in low-income countries.
Write to gh@ideas42.org if you’re interested in exploring how these approaches could be applied to your setting.


